Connect With Us
Blog

Treat Cracked Heels This Fall With the Help of Your Podiatrist
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
What Causes Plantar Fasciitis?
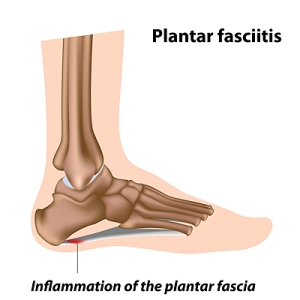
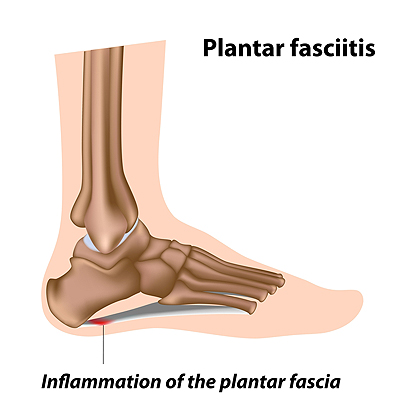 The plantar fascia is the band of tissue that run along the bottom of the foot and connects the heel to the toes. When the plantar fascia becomes inflamed or partially torn, it results in the condition that is commonly referred to as plantar fasciitis. Plantar fasciitis is one of the most common causes of heel pain. The pain is usually worse in the morning and after long periods of rest. Common causes of plantar fasciitis includes sitting or standing for long periods of time, having tight calf muscles, having flat feet or high arches, obesity, and arthritis. Patients who are struggling with heel pain should consult with a podiatrist because there are a variety of causes. Once you visit with a podiatrist, they will be able to provide a proper diagnosis, as well as a customized treatment plan for your condition.
The plantar fascia is the band of tissue that run along the bottom of the foot and connects the heel to the toes. When the plantar fascia becomes inflamed or partially torn, it results in the condition that is commonly referred to as plantar fasciitis. Plantar fasciitis is one of the most common causes of heel pain. The pain is usually worse in the morning and after long periods of rest. Common causes of plantar fasciitis includes sitting or standing for long periods of time, having tight calf muscles, having flat feet or high arches, obesity, and arthritis. Patients who are struggling with heel pain should consult with a podiatrist because there are a variety of causes. Once you visit with a podiatrist, they will be able to provide a proper diagnosis, as well as a customized treatment plan for your condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Mack Jay Groves IV, DPM from Practice. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Covington, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
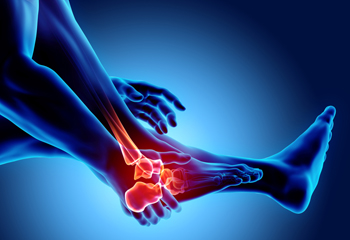
When to Get Help for Ankle Pain
Ankle pain has many potential causes, ranging from simple fatigue to serious injuries. Sometimes it can be difficult to determine when you should manage your ankle pain at home and when you should seek medical care since ankle pain and accompanying symptoms may start out mild and worsen over time. Pay close attention to your symptoms. You should see a podiatrist if the ankle is misshapen, the calf is hot, swollen, or tender, or if you have difficulty putting weight on your leg. You should also schedule an appointment with a podiatrist if you have ankle pain that is worsening. If there is significant trauma to the ankle, it is imperative that you seek the care of a podiatrist immediately.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Mack Jay Groves IV, DPM from Practice. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Covington, LA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Foot Joint Deformities in Rheumatoid Arthritis
Joint deformities are sometimes a complication of rheumatoid arthritis (RA). Fortunately, joint deformities are becoming less common thanks to early detection and treatment. Nevertheless, it is helpful to be aware of joint deformity caused by RA and what can be done to treat it. The most common types of joint deformities in the feet of people with RA are claw, mallet, and hammertoes. People with these deformities have toes that are stuck in a bent position at one of the toe joints. These conditions can be treated through the use of orthotic devices, such as insoles or splints, or with surgery. If you have RA, it is suggested that you are under the care of a podiatrist who can help you maintain your foot health.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Mack Jay Groves IV, DPM of Practice. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Covington, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
How to Buy Shoes That Fit You
Happy feet start with shoes that are comfortable and fit well. When purchasing shoes, do your shopping in the afternoon when your feet are usually their largest. Have your feet measured every time to make sure your size has not changed, as can happen over time. If you are like most people, one foot will be slightly larger than the other; choose the size that accommodates the larger foot. Ensure that the ball of your foot fits the widest part of the shoe comfortably. Check the length of the shoe to make sure there is ample room for your toes, and choose shoes that are shaped similarly to your feet. Remember that shoe sizes can fluctuate based on brand and other factors, so always try them on. While standing, check to make sure the width of your finger fits comfortably between the top of your toes and the tip of the shoe. Walk around the store to make sure they feel good and do not slip or rub you uncomfortably. If the shoes do not feel great in the store, don’t rely on them stretching out with wear. A podiatrist can make other specific recommendations based on your foot structure and needs, and also provide custom orthotics for additional support, or to correct any gait issues you may have.
Finding a properly-fitting shoe is important in reducing injuries and preventing foot problems. For more information about treatment, contact Mack Jay Groves IV, DPM from Practice. Our doctor will treat your foot and ankle needs.
Proper Shoe Fitting
A common concern when it comes to foot health, having properly fitted shoes can help prevent injuries to the foot. Out feet affect our posture and gait, which in turn affects the biomechanics and overall bodily structure. With 33 joints, 26 bones, and over 100 ligaments, the potential for serious injury is much greater than one realizes. Although the feet cease growth in adulthood, they still change shape as they mature. Here are some factors to consider when it comes to investing in proper fitting shoes:
- Be sure the shoes fit correctly right away
- Ensure the ball of your foot fits comfortably in the widest portion of the shoes
- Even though they may look fashionable, improper fitting shoes can either create adverse conditions or exacerbate existing ones you may already have
- Walk along a carpeted surface to ensure the shoes comfortably fit during normal activity
Keeping in mind how shoes fit the biomechanics of your body, properly-fitting shoes are vitally important. Fortunately, it is not difficult to acquire footwear that fits correctly. Be sure to wear shoes that support the overall structure of your body. Do your feet a favor and invest in several pairs of well-fitted shoes today.
If you have any questions please feel free to contact our office located in Covington, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.